Disruptions from Babylon Health’s app are spreading through the U.K.’s National Health Service, with its AI, virtual services and promise of appointments “just a tap away.” But will it go too far, and threaten the funding of the government health system?
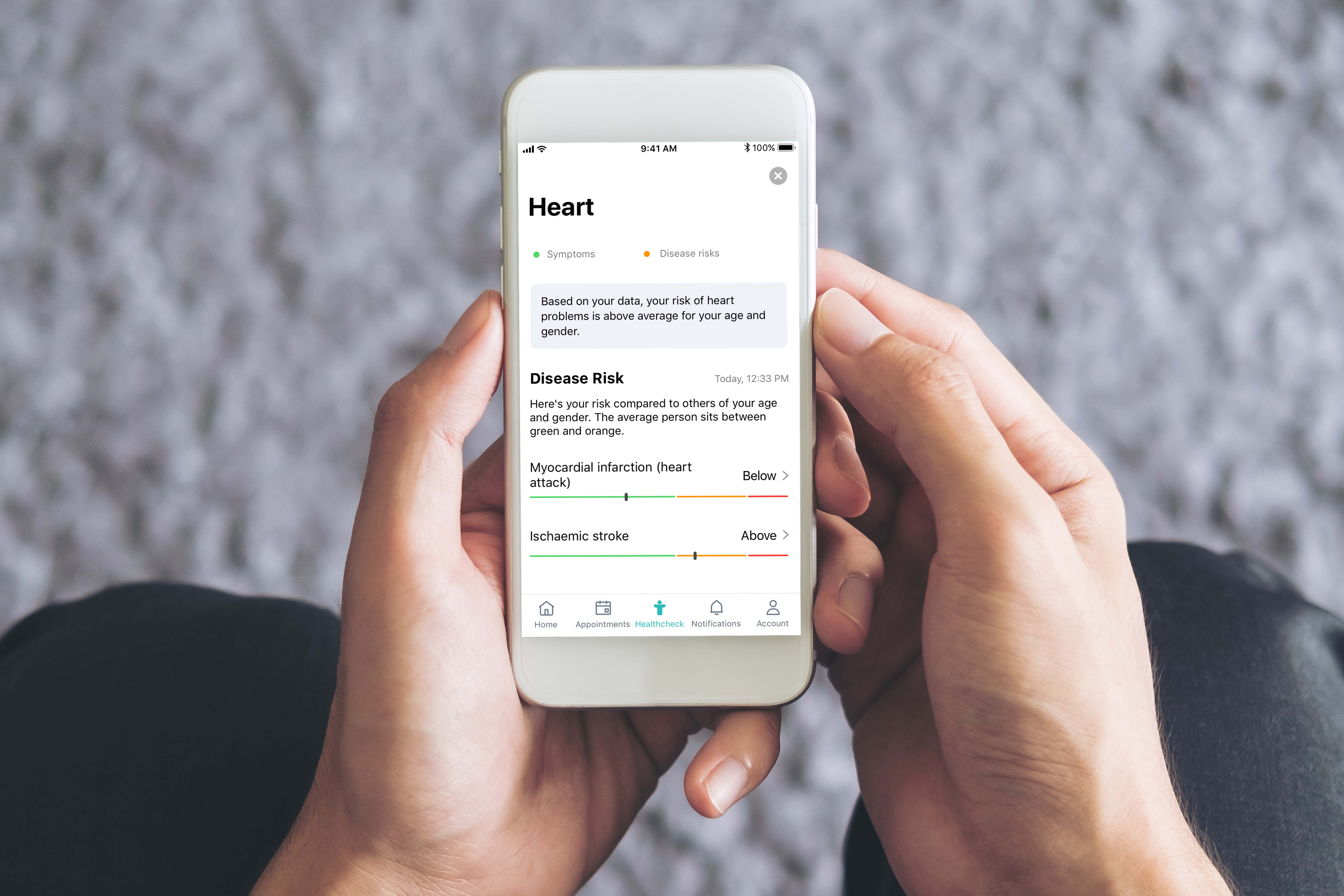
With Britain’s NHS, users visit their local general practitioner before accessing most hospital or other care services, which adds travel and long waits. Babylon created its “GP at Hand” app to cut through that.
On paper, the firm is the same as every other practice. When new patients register they leave their old GP and then make appointments to speak to Babylon’s doctors and access its healthcare services. The big difference is that Babylon will accept patients across a wide area instead of being rooted in one building in one region.
This permits Babylon to make GP appointments with less hassle. There are also efficiencies in how doctors spend their time, since working virtually means they can work from anywhere too. The company manages some physical offices for when patients require services that cannot be delivered virtually, such as vaccinations or blood tests.
Founded by former investment banker Ali Parsa in 2013, the service has been wildly successful. The company says that it has signed up 50,000 patients to use its services in London and Birmingham alone, and it is looking to expand into services to other localities and even to other countries, having already opened offices in the U.S., Canada, Singapore, Malaysia and Rwanda.
Investors have taken notice. In April 2017, it raised $60 million, with reported contributors including Egyptian billionaire Nassef Sawiris, valuing the company at $100 million. In January 2016, its Series A round of funding $25 million, with investors including Hoxton Ventures and the founders of Google’s DeepMind.
NHS Stress Test
There is a backlash to the company’s success. The problem isn’t that the upstart is using new technology – the problem is that it is breaking the existing NHS funding model with two structural challenges.
The way funding works is that GPs receive income via regional Clinical Commission Groups (CCGs), which they fund all of the GPs in a given locality – even if registered patients live outside of the area. This means that, as noted by Wired, Hammersmith and Fulham CCG, where Babylon happens to be based, ends up being on the hook for paying for the many thousands of Babylon patients who are based elsewhere, rather than the handful of outside patients that would be expected in a traditional GP practice.
The other challenge is one of demographics: In 2017 the average GP received about $188 per patient. But obviously the cash would be distributed unevenly, with healthy, younger people contributing cash that could be spent on people who are older with more complex needs.
Unsurprisingly, this younger demographic are the ones being lured away by Babylon – leaving traditional GPs with a funding blackhole and the most difficult patients to deal with.
The company has also faltered in its aspirations. In 2018, it failed to land the $400 million of funding it was seeking in talks with Softbank, according to Algorithm X Lab, and the company is still spending more money than it makes: reportedly its workforce costs the company $75 million but are only generating revenue of $10 million. The Financial Times reported this year that its fundraising efforts were continuing as it burns through cash.
Given how aggressively Babylon is expanding, into both new products and new markets, it is surely inevitable that video consultations and AI triage will become an increasingly prominent part of the future of the NHS




















![Michael Halen: “The [restaurant] industry is very far behind…when it comes to investments in technology.”](/wp-content/uploads/2019/08/art-card-ceramic-cup-1001990-696x385.jpg)



